Folic acid (the anion form is called folate) is a B-complex vitamin (once called vitamin M) that is important in preventing neural tube defects (NTDs) in the developing human fetus.
Folic acid and pregnancy
Since the discovery of the link between insufficient folic acid and NTDs, governments and health organisations worldwide have made recommendations concerning folic acid supplementation for women intending to become pregnant. For example, the US Public Health service (see the URL given at page foot) recommends an extra 0.4mg/day, which can be taken as a pill. However, many researchers believe that supplementation in this way can never work effectively enough since not all pregnancies are planned and not all women will comply with the recommendation.
This has led to the introduction in many countries of fortification, where folic acid is added to flour with the intention of everyone benefiting from the associated raise in blood folate levels. This is not uncontroversial, with issues having been raised concerning individual liberty, and the masking effect of folate fortification on B12 deficiency or pernicious anaemia. However, most North and South American countries now fortify their flour, along with a number of Middle Eastern countries and Indonesia. Mongolia and a number of ex-Soviet republics are amongst those having widespread voluntary fortification; about five more countries (including Morocco, the first African country) have agreed but not yet implemented fortification. The UK has recently decided not to fortify, mainly because of the B12 concern; indeed, no EU country has yet fortified.
Although folic acid does reduce the risk of birth defects, it is only one part of the picture and should not be considered a cure. Even women taking daily folic acid supplements have been known to have children with neural tube defects.
Folic acid and ischaemic heart disease
Recent research also points out a further benefit of folic acid: that it can help lower levels of homocysteine. High levels of homocysteine are statistically associated with a risk of ischaemic heart disease (IHD). At this time, though, there is no proof of cause and effect and as the AHA (http://www.americanheart.org/presenter.jhtml?identifier=4677) says:
- The American Heart Association has not yet called hyperhomocysteinemia (hi"per-ho"mo-sis-TE'in-E'me-ah) (high homocysteine level) a major risk factor for cardiovascular disease. We don't recommend widespread use of folic acid and B vitamin supplements to reduce the risk of heart disease and stroke. We advise a healthy, balanced diet that includes five servings of fruits and vegetables a day.
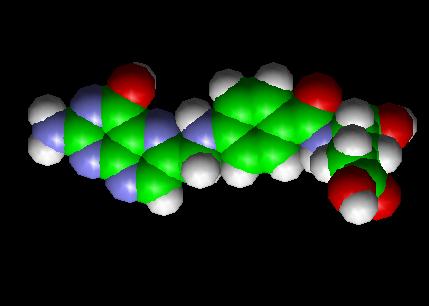
Biochemistry
In the form of a series of tetrahydrofolate compounds, folate derivatives are coenzymes in a number of single carbon transfer reactions biochemically, and also is involved in the synthesis of dTMP (2'-deoxythymidine-5'-phosphate) from dUMP (2'-deoxyuridine-5'-phosphate).
The pathway in the formation of tetrahydrofolate (FH4) is the reduction of folate (F) to dihydrofolate (FH2) by folate reductase, and then the subsequent reduction of dihydrofolate to tetrahydrofolate (FH4) by dihydrofolate reductase.
Methylene tetrahydrofolate (CH2=FH4) is formed from tetrahydrofolate by the addition of methylene groups from one of three carbon donors: formaldehyde, serine, or glycine. Methyl tetrahydrofolate (CH3-FH4) can be made from methylene tetrahydrofolate by reduction of the methylene, and methylidine tetrahydrofolate (CHO-FH4) is made by oxidation of the methylene tetrahydrofolate.
A number of drugs interfere with the biosynthesis of folic acid and tetrahydrofolate. Among them are the antibiotics trimethoprim (which acts on dihydrofolate reductase), the sulfonamides (competitive inhibitors of para-aminobenzoic acid in the reactions of dihydropteroate synthetase), the antimalarial pyrimethamine, and the anticancer drug methotrexate (inhibits both folate reductase and dihydrofolate reductase).
Folate and folic acid are forms of a water-soluble B vitamin. Folate occurs naturally in food. Folic acid is the synthetic form of this vitamin that is found in supplements and fortified foods (1). Folate gets its name from the Latin word "folium" for leaf. A key observation of researcher Lucy Wills nearly 70 years ago led to the identification of folate as the nutrient needed to prevent the anemia of pregnancy. Dr. Wills demonstrated that the anemia could be corrected by a yeast extract. Folate was identified as the corrective substance in yeast extract in the late 1930s and was extracted from spinach leaves in 1941. Folate is necessary for the production and maintenance of new cells (2). This is especially important during periods of rapid cell division and growth such as infancy and pregnancy. Folate is needed to make DNA and RNA, the building blocks of cells. It also helps prevent changes to DNA that may lead to cancer (3). Both adults and children need folate to make normal red blood cells and prevent anemia (4).
Folate in foods
Leafy greens such as spinach and turnip greens, dry beans and peas, fortified cereals and grain products, and some fruits and vegetables are rich food sources of folate. Some breakfast cereals (ready-to-eat and others) are fortified with 25 percent or 100 percent of the Daily Value (DV) for folic acid. The table of selected food sources of folate and folic acid suggests dietary sources of this vitamin (5). In 1996, the Food and Drug Administration (FDA) published regulations requiring the addition of folic acid to enriched breads, cereals, flours, corn meals, pastas, rice, and other grain products (6-8). This ruling took effect January 1, 1998, and was specifically targeted to reduce the risk of neural tube birth defects in newborns (9). Since the folic acid fortification program took effect, fortified foods have become a major source of folic acid in the American diet. Synthetic folic acid that is added to fortified foods and dietary supplements has a simpler chemical structure than the natural form of folate, and is absorbed more easily by the body. After digestion and absorption however, the two forms are identical and function in exactly the same manner.
Recommended Dietary Allowance for folate
The Recommended Dietary Allowance (RDA) is the average daily dietary intake level that is sufficient to meet the nutrient requirements of nearly all (97 to 98 percent) healthy individuals in each life-stage and gender group (10). The 1998 RDAs for folate are expressed in a term called the Dietary Folate Equivalent. The Dietary Folate Equivalent (DFE) was developed to help account for the differences in absorption of naturally occurring dietary folate and the more bioavailable synthetic folic acid (11). The 1998 RDAs for folate expressed in micrograms (mcg) of DFE for adults are (10):
Life Stage Men Women Pregnancy Lactation Ages 19+ 400 mcg 400 mcg All ages 600 mcg 500 mcg
1 mcg of food folate = 0.6 mcg folic acid from supplements and fortified foods
The National Health and Nutrition Examination Survey (NHANES III 1988-91) and the Continuing Survey of Food Intakes by Individuals (1994-96 CSFII) indicated that most adults did not consume adequate folate (10, 12, 13). However, the folic acid fortification program has increased folic acid content of commonly eaten foods such as cereals and grains, and as a result diets of most adults now provide recommended amounts of folate equivalents (14).
Folate deficiency
A deficiency of folate can occur when your need for folate is increased, when dietary intake of folate is inadequate, and when your body excretes (or loses) more folate than usual. Medications that interfere with your body's ability to use folate may also increase the need for this vitamin (1, 6, 15 -19). Some situations that increase the need for folate include:
- pregnancy and lactation (breastfeeding)
- alcohol abuse
- malabsorption
- kidney dialysis
- liver disease
- certain anemias.
Medications can interfere with folate utilization, including:
- anti-convulsant medications (such as dilantin, phenytoin, and primidone) Metformin (sometimes prescribed to control blood sugar in type 2 diabetes)
- Sulfasalazine (used to control inflammation associated with Crohn's disease and ulcerative colitis)
- Triamterene (a diuretic)
- Methotrexate.
Signs of folate deficiency
Signs of folic acid deficiency are often subtle. Diarrhea, loss of appetite, and weight loss can occur. Additional signs are weakness, sore tongue, headaches, heart palpitations, irritability, and behavioral disorders (1, 20). Women with folate deficiency who become pregnant are more likely to give birth to low birth weight and premature infants, and infants with neural tube defects. In adults, anemia is a sign of advanced folate deficiency. In infants and children, folate deficiency can slow growth rate. Some of these symptoms can also result from a variety of medical conditions other than folate deficiency. It is important to have a physician evaluate these symptoms so that appropriate medical care can be given.
Who may need extra folic acid to prevent a deficiency?
Women of childbearing age, people who abuse alcohol, anyone taking anti-convulsants or other medications that interfere with the action of folate, individuals diagnosed with anemia from folate deficiency, and individuals with malabsorption, liver disease, or who are receiving kidney dialysis treatment may benefit from a folic acid supplement.
Folic acid is very important for all women who may become pregnant. Adequate folate intake during the periconceptual period, the time just before and just after a woman becomes pregnant, protects against a number of congenital malformations including neural tube defects (21). Neural tube defects result in malformations of the spine (Spina bifida), skull, and brain (anencephaly) (10). The risk of neural tube defects is significantly reduced when supplemental folic acid is consumed in addition to a healthful diet prior to and during the first month following conception (5, 22, 23). Women who could become pregnant are advised to eat foods fortified with folic acid or take supplements in addition to eating folate-rich foods to reduce the risk of some serious birth defects. Taking 400 micrograms of synthetic folic acid daily from fortified foods and/or supplements has been suggested (10). The Recommended Dietary Allowance (RDA) for folate equivalents for pregnant women is 600 micrograms (10).
Folate deficiency has been observed in alcoholics. A 1997 review of the nutritional status of chronic alcoholics found low folate status in more than 50 percent of those surveyed (24). Alcohol interferes with the absorption of folate and increases excretion of folate by the kidney. In addition, many alcohol abusers have poor quality diets that do not provide the recommended intake of folate (17). Increasing folate intake through diet, or folic acid intake through fortified foods or supplements, may be beneficial to the health of alcoholics.
Anti-convulsant medications such as dilantin increase the need for folate (25,26). Anyone taking anti-convulsants and other medications that interfere with the body's ability to use folate should consult with a medical doctor about the need to take a folic acid supplement (27-29).
Anemia is a condition that occurs when red blood cells cannot carry enough oxygen. It can result from a wide varietyof medical problems, including folate deficiency. Folate deficiency can result in the formation of large red blood cells that do not contain adequate hemoglobin, the substance in red blood cells that carries oxygen to your body's cells (4). Your physician can determine whether an anemia is associated with folate deficiency and whether supplemental folic acid is indicated.
Several medical conditions increase the risk of folic acid deficiency. Liver disease and kidney dialysis increase excretion (loss) of folic acid. Malabsorption can prevent your body from using folate in food. Medical doctors treating individuals with these disorders will evaluate the need for a folic acid supplement (1).
Caution about folic acid supplements
Beware of the interaction between vitamin B12 and folic acid. Folic acid supplements can correct the anemia associated with vitamin B12 deficiency. Unfortunately, folic acid will not correct changes in the nervous system that result from vitamin B12 deficiency. Permanent nerve damage can occur if vitamin B12 deficiency is not treated. Intake of supplemental folic acid should not exceed 1,000 micrograms (mcg) per day to prevent folic acid from masking symptoms of vitamin B12 deficiency (10).
It is very important for older adults to be aware of the relationship between folic acid and vitamin B12 because they are at greater risk of having a vitamin B12 deficiency. If you are 50 years of age or older, ask your physician to check your B12 status before you take a supplement that contains folic acid.
Folic acid and heart disease
A deficiency of folate, vitamin B12, or vitamin B6 may increase your level of homocysteine, an amino acid normally found in your blood. There is evidence that an elevated homocysteine level is an independent risk factor for heart disease and stroke (30 - 41). The evidence suggests that high levels of homocysteine may damage coronary arteries or make it easier for blood clotting cells called platelets to clump together and form a clot (36). However, there is currently no evidence available to suggest that lowering homocysteine with vitamins will reduce your risk of heart disease. Clinical intervention trials are needed to determine whether supplementation with folic acid, vitamin B12 or vitamin B6 can lower your risk of developing coronary heart disease.
Folic acid and cancer
Some evidence associates low blood levels of folate with a greater risk of cancer (42). Folate is involved in the synthesis, repair, and functioning of DNA, our genetic map, and a deficiency of folate may result in damage to DNA that may lead to cancer (43). Several studies have associated diets low in folate with increased risk of breast, pancreatic, and colon cancer (44, 45). Findings from a study of over 121,000 nurses suggested that long-term folic acid supplementation (for 15 years) was associated with a decreased risk of colon cancer in women aged 55 to 69 years of age (44). However, associations between diet and disease do not indicate a direct cause. Researchers are continuing to investigate whether enhanced folate intake from foods or folic acid supplements may reduce the risk of cancer. Until results from such clinical trials are available, folic acid supplements should not be recommended to reduce the risk of cancer.
Folic acid and methotrexate for cancer
Folate is important for cells and tissues that rapidly divide (2). Cancer cells divide rapidly, and drugs that interfere with folate metabolism are used to treat cancer. Methotrexate is a drug often used to treat cancer because it limits the activity of enzymes that need folate. Unfortunatley, methotrexate can be toxic (46-48), producing side effects such as inflammation in the digestive tract that make it difficult to eat normally. Leucovorin is a form of folate that can help "rescue" or reverse the toxic effects of methotrexate (49). It is not known whether folic acid supplements can help control the side effects of methotrexate without decreasing its effectiveness in chemotherapy (50-51). It is important for anyone receiving methotrexate to follow a medical doctor's advice on the use of folic acid supplements.
Folic acid and methotrexate for non-cancerous diseases
Low dose methotrexate is used to treat a wide variety of non-cancerous diseases such as rheumatoid arthritis, lupus, psoriasis, asthma, sarcoidoisis, primary biliary cirrhosis, and inflammatory bowel disease (52). Low doses of methotrexate can deplete folate stores and cause side effects that are similar to folate deficiency. Both high folate diets and supplemental folic acid may help reduce the toxic side effects of low dose methotrexate without decreasing its effectiveness, (53, 54). Anyone taking low dose methotrexate for the health problems listed above should consult with a physician about the need for a folic acid supplement.
What is the health risk of too much folic acid?
The risk of toxicity from folic acid is low (55). The Institute of Medicine has established a tolerable upper intake level (UL) for folate of 1,000 mcg for adult men and women, and a UL of 800 mcg for pregnant and lactating (breast-feeding) women less than 18 years of age (10). Supplemental folic acid should not exceed the UL to prevent folic acid from masking symptoms of vitamin B12 deficiency (10, 29).
Selected food sources of folate and folic acid
As the 2000 Dietary Guidelines for Americans states, "Different foods contain different nutrients and other healthful substances. No single food can supply all the nutrients in the amounts you need" (56). The following table suggests dietary sources of folate. As the table indicates, green leafy vegetables, dry beans and peas, and many other types of vegetables and fruits are good sources of folate. In addition, fortified foods are a major source of folic acid. It is not unusual to find foods such as cereals fortified with 100 percent of the RDA for folate. The variety of fortified foods available has made it easier for women of childbearing age to consume the recommended 400 mcg of folic acid per day from fortified foods and/or supplements (6). The large numbers of fortified foods on the market, however, also raise concern that intake may exceed the UL. This is especially important for anyone at risk of vitamin B12 deficiency, which can be masked by too much folic acid. It is important for anyone who is considering taking a folic acid supplement to first consider whether their needs are being met by adequate sources of dietary folate and folic acid from fortified foods. If you want more information about building a healthful diet, refer to the Dietary Guidelines for Americans and the Food Guide Pyramid.
References
1. Herbert V. Folic Acid. In: Shils M, Olson J, Shike M, Ross AC, ed. Nutrition in Health and Disease. Baltimore: Williams & Wilkins, 1999.
2. Kamen B. Folate and antifolate pharmacology. Semin Oncol 1997; 24:S18-30-S18-39.
3. Fenech M, Aitken C, Rinaldi J. Folate, vitamin B12, homocysteine status and DNA damage in young Australian adults. Carcinogenesis 1998; 19:1163-71.
4. Zittoun J. Anemias due to disorder of folate, vitamin B12 and transcobalamin metabolism. Rev Prat 1993; 43:1358-63.
5. U.S. Department of Agriculture, Agricultural Research Service,1999. USDA Nutrient Database for Standard Reference, Release 13. Nutrient Data Lab Home Page, http://www.nal.usda.gov/fnic/foodcomp
6. Oakley GP, Jr., Adams MJ, Dickinson CM. More folic acid for everyone, now. J Nutr 1996; 126:751S-755S.
7. Malinow MR, Duell PB, Hess DL, Anderson PH, Kruger WD, Phillipson BE, Gluckman RA, Upson BM. Reduction of plasma homocyst(e)ine levels by breakfast cereal fortified with folic acid in patients with coronary heart disease. N Engl J Med 1998; 338:1009-15.
8. Daly S, Mills JL, Molloy AM, Conley M, Lee YJ, Kirke PN, Weir DG, Scott JM. Minimum effective dose of folic acid for food fortification to prevent neural-tube defects. Lancet 1997; 350:1666-9.
9. Crandall BF, Corson VL, Evans MI, Goldberg JD, Knight G, Salafsky IS. American College of Medical Genetics statement on folic acid: Fortification and supplementation. Am J Med Genet 1998; 78:381.
10. Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes: Thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, pantothenic Acid, biotin, and choline. National Academy Press. Washington, DC, 1998.
11. Suitor CW and Bailey LB. Dietary folate equivalents: Interpretation and application. J Am Diet Assoc 2000; 100:88-94.
12. Raiten DJ and Fisher KD. Assessment of folate methodology used in the Third National Health and Nutrition Examination Survey (NHANES III, 1988-1994). J Nutr 1995; 125:1371S-1398S.
13. Alaimo K, McDowell MA, Briefel RR, Bischlf AM, Caughman CR, Loria CM, Johnson CL. Dietary Intake of Vitamins, Minerals, and Fiber of Persons Ages 2 Months and Over in the United States: Third National Health and Nutrition Examination Survey, Phase 1, 1988-91. In: Johnson GV, ed. Hyattsville, MD: Vital and Health Statistics of the Center for Disease Control and Prevention/National Center for Health Statistics, 1994:1-28.
14. Lewis CJ, Crane NT, Wilson DB, Yetley EA. Estimated folate intakes: Data updated to reflect food fortification, increased bioavailability, and dietary supplement use. Am J Clin Nutr 1999; 70:198-207.
15. McNulty H. Folate requirements for health in different population groups. Br J Biomed Sci 1995;52:110-9.
16. Stolzenberg R. Possible folate deficiency with postsurgical infection. Nutr Clin Pract 1994;9:247-50.
17. Cravo ML, Gloria LM, Selhub J, Nadeau MR, Camilo ME, Resende MP, Cardoso JN, Leitao CN, Mira FC. Hyperhomocysteinemia in chronic alcoholism: Correlation with folate, vitamin B-12, and vitamin B-6 status. Am J Clin Nutr 1996; 63:220-4.
18. Pietrzik KF and Thorand B. Folate economy in pregnancy. Nutrition 1997;13:975-7.
19. Kelly GS. Folates: Supplemental forms and therapeutic applications. Altern Med Rev 1998; 3:208-20.
20. Haslam N and Probert CS. An audit of the investigation and tre
atment of folic acid deficiency. J R Soc Med 1998; 91:72-3.
21. Shaw GM, Schaffer D, Velie EM, Morland K, Harris JA. Periconceptional vitamin use, dietary folate, and the occurrence of neural tube defects. Epidemiology 1995; 6:219-226.
22. Mulinare J, Cordero JF, Erickson JD, Berry RJ. Periconceptional use of multivitamins and the occurrence of neural tube defects. J Am Med Assoc 1988; 260:3141-3145.
23 Milunsky A, Jick H, Jick SS, Bruell CL, MacLaughlin DS, Rothman KJ, Willett W. Multivitamin/folic acid supplementation in early pregnancy reduces the prevalence of neural tube defects. J Am Med Assoc 1989; 262:2847-2852.
24. Gloria L, Cravo M, Camilo ME, Resende M, Cardoso JN, Oliveira AG, Leitao CN, Mira FC. Nutritional deficiencies in chronic alcoholics: Relation to dietary intake and alcohol consumption. Am J Gastroenterol 1997; 92:485-9. 25. Collins CS, Bailey LB, Hillier S, Cerda JJ, Wilder BJ. Red blood cell uptake of supplemental folate in patients on anticonvulsant drug therapy. Am J Clin Nutr 1988; 48:1445-1450.
26. Young SN and Ghadirian AM. Folic acid and psychopathology. Prog Neuropsychopharmacol Biol Psychiat 1989; 13:841-863.
27. Munoz-Garcia D, Del Ser T, Bermejo F, Portera A. Truncal ataxia in chronic anticonvulsant treatment. Association with drug-induced folate deficiency. J Neurol Sci 1982; 55:305-11.
28. Eller DP, Patterson CA, Webb GW. Maternal and fetal implications of anticonvulsive therapy during pregnancy. Obstet Gynecol Clin North Am 1997; 24:523-34.
29. Baggott JE, Morgan SL, HaT, Vaughn WH, Hine RJ. Inhibition of folate-dependent enzymes by non-steroidal anti-imflammatory drugs. Biochem 1992; 282:197-202.
30. Selhub J, Jacques PF, Bostom AG, D'Agostino RB, Wilson PW, Belanger AJ, O'Leary DH, Wolf PA, Scaefer EJ, Rosenberg IH. Association between plasma homocysteine concentrations and extracranial carotid-artery stenosis. N Engl J Med 1995; 332:286-291.
31. Rimm EB, Willett WC, Hu FB, Sampson L, Colditz GA, Manson JE, Hennekens C, Stampfer MJ. Folate and vitamin B6 from diet and supplements in relation to risk of coronary heart disease among women. J Am Med Assoc 1998;279:359-64.
32. Refsum H, Ueland PM, Nygard O, Vollset SE. Homocysteine and cardiovascular disease. Annu Rev Med 1998; 49:31-62.
33. Boers GH. Hyperhomocysteinaemia: A newly recognized risk factor for vascular disease. Neth J Med 1994; 45:34-41. 34. Selhub J, Jacque PF, Wilson PF, Rush D, Rosenberg IH. Vitamin status and intake as primary determinants of homocysteinemia in an elderly population. J Am Med Assoc 1993 ;270:2693-2698.
35. Mayer EL, Jacobsen DW, Robinson K. Homocysteine and coronary atherosclerosis. J Am Coll Cardiol 1996; 27:517-27.
36. Malinow MR. Plasma homocyst(e)ine and arterial occlusive diseases: A mini-review. Clin Chem 1995; 41:173-6.
37. Flynn MA, Herbert V, Nolph GB, Krause G. Atherogenesis and the homocysteine-folate-cobalamin triad: Do we need standardized analyses? J Am Coll Nutr 1997; 16:258-67.
38. Fortin LJ and Genest J, Jr. Measurement of homocyst(e)ine in the prediction of arteriosclerosis. Clin Biochem 1995; 28:155-62.
39. Siri PW, Verhoef P, Kok FJ. Vitamins B6, B12, and folate: Association with plasma total homocysteine and risk of coronary atherosclerosis. J Am Coll Nutr 1998; 17:435-41.
40. Eskes TK. Open or closed? A world of difference: A history of homocysteine research. Nutr Rev 1998; 56:236-44.
41. Ubbink JB, van der Merwe A, Delport R, Allen RH, Stabler SP, Riezler R, Vermaak WJ. The effect of a subnormal vitamin B-6 status on homocysteine metabolism. J Clin Invest 1996; 98:177-84.
42. Freudenheim JL, Grahm S, Marshall JR, Haughey BP, Cholewinski S, Wilkinson G. Folate intake and carcinogenesis of the colon and rectum. Int J Epidemiol 1991; 20:368-374. 43. Jennings E. Folic acid as a cancer preventing agent. Med Hypothesis 1995; 45:297-303.
44. Christensen B. Folate deficiency, cancer and congenital abnormalities. Is there a connection? . Tidsskr Nor Laegeforen 1996; 116:250-4.
45. Giovannucci E, Stampfer MJ, Colditz GA, Hunter DJ, Fuchs C, Rosner BA, Speizer FE, Willett WC. Multivitamin use, folate, and colon cancer in women in the Nurses' Health Study. Ann Intern Med 1998; 129:517-524.
46. Rubio IT, Cao Y, Hutchins LF, Westbrook KC, Klimberg VS. Effect of glutamine on methotrexate efficacy and toxicity. Ann Surg 1998; 227:772-8.
47. Wolff JE, Hauch H, Kuhl J, Egeler RM, Jurgens H. Dexamethasone increases hepatotoxicity of MTX in children with brain tumors. Anticancer Res 1998; 18:2895-9.
48. Kepka L, De Lassence A, Ribrag V, Gachot B, Blot F, Theodore C, Bonnay M, Korenbaum C, Nitenberg G. Successful rescue in a patient with high dose methotrexate-induced nephrotoxicity and acute renal failure. Leuk Lymphoma 1998; 29:205-9.
49. Branda RF, Nigels E, Lafayette AR, Hacker M. Nutritional folate status influences the efficacy and toxicity of chemotherapy in rats. Blood 1998; 92:2471-6.
50. Shiroky JB. The use of folates concomitantly with low-dose pulse methotrexate. Rheum Dis Clin North Am 1997;23:969-80.
51. Keshava C, Keshava N, Whong WZ, Nath J, Ong TM. Inhibition of methotrexate-induced chromosomal damage by folinic acid in V79 cells. Mutat Res 1998; 397:221-8.
52. Morgan SL and Baggott JE. Folate antagonists in nonneoplastic disease: Proposed mechanisms of efficacy and toxicity. In: Bailey LB, ed. Folate in Health and Disease. New York: Marcel Dekker, 1995: 405-433.
53. Morgan SL BJ, Alarcon GS. Methotrexate in rheumatoid arthritis. Folate supplementation should always be given. Bio Drugs 1997; 8:164-175.
54. Morgan SL, Baggott JE, Lee JY, Alarcon GS. Folic acid supplementation prevents deficient blood folate levels and hyperhomocysteinemia during longterm, low dose methotrexate therapy for rheumatoid arthritis: Implications for cardiovascular disease prevention. J Rheumatol 1998; 25:441-6. 55. Hathcock JN. Vitamins and minerals: Efficacy and safety. Am J Clin Nutr 1997;66:427-37. 56. Dietary Guidelines Advisory Committee, Agricultural Research Service, United States Department of Agriculture (USDA). Report of the Dietary Guidelines AdvisoryCommittee on the Dietary Guidelines for Americans, 2000. http://www.ars.usda.gov/dgac
External Links
- Health Canada article about folic acid (http://www.hc-sc.gc.ca/english/iyh/medical/folic_acid.html)
- US Public Health Service information page on folic acid (http://www.cdc.gov/ncbddd/folicacid/)
- http://www.nobel.se/medicine/laureates/1988/hitchings-lecture.pdf
- BMJ Editorial - "Delaying folic acid fortification of flour" (http://bmj.com/cgi/content/full/324/7350/1348)
- Folate Information (http://www.talkwellness.org/folate.html)
This article contains information from the public domain resource at http://www.cc.nih.gov/ccc/supplements/folate.html