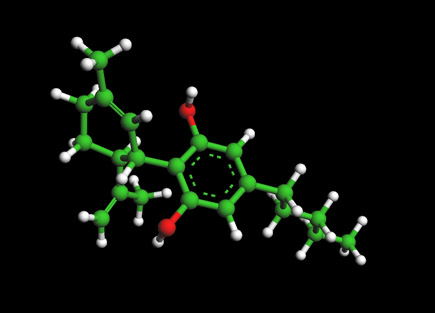
Lipitor Molecule - Atorvastatin

Ball and Stick Model for Molecule - Lipitor Molecule -Atorvastatin
To View the Lipitor Molecule in 3D --->>in 3D with Jsmol
Atorvastatin marketed under the trade name Lipitor and several others, is a member of the drug class known as statins, used for lowering cholesterol. Atorvastatin inhibits the rate-determining enzyme located in hepatic tissue that produces mevalonate, a small molecule used in the synthesis of cholesterol and other mevalonate derivatives. This lowers the amount of cholesterol produced which in turn lowers the total amount of LDL cholesterol. With 2006 sales of US$12.9 billion under the brand name Lipitor, it is the largest selling drug in the world.[1] Lipitor is not the only statin. There are over 5 other statins in the market.[2][3]
Statins currently available on the U.S. market include: Lipitor (atorvastatin) - Pfizer Zocor (simvastatin) - Merck Pravachol (pravastatin) - Bristol-Myers Squibb Lescol (fluvastatin) - Novartis Mevacor (lovastatin) - Merck Crestor (rosuvastatin) - AstraZeneca.
The statins (or HMG-CoA reductase inhibitors) form a class of hypolipidemic drugs used to lower cholesterol levels in people with or at risk of cardiovascular disease. They lower cholesterol by inhibiting the enzyme HMG-CoA reductase, which is the rate-limiting enzyme of the mevalonate pathway of cholesterol synthesis. Inhibition of this enzyme in the liver stimulates LDL receptors, resulting in an increased clearance of low-density lipoprotein (LDL) from the bloodstream and a decrease in blood cholesterol levels. The first results can be seen after one week of use and the effect is maximal after four to six weeks.
Pharmacology
As with other statins, atorvastatin is a competitive inhibitor of HMG-CoA reductase. Unlike most others, however, it is a completely synthetic compound. HMG-CoA reductase catalyzes the reduction of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) to mevalonate, which is the rate-limiting step in hepatic cholesterol biosynthesis. Inhibition of the enzyme decreases de novo cholesterol synthesis, increasing expression of low-density lipoprotein receptors (LDL receptors) on hepatocytes. This increases LDL uptake by the hepatocytes, decreasing the amount of LDL-cholesterol in the blood. Like other statins, atorvastatin also reduces blood levels of triglycerides and slightly increases levels of HDL-cholesterol.
In clinical trials, adding ezetimibe (Zetia) to Lipitor lowered cholesterol more effectively than Vytorin (ezetimibe + simvastatin).
Clinical use
Indications
Atorvastatin is indicated as an adjunct to diet for the treatment of dyslipidemia, specifically hypercholesterolaemia. It has also been used in the treatment of combined hyperlipidemia.[4]
In 2005, the PROVE IT-TIMI 22 trial compared 40mg/day pravastatin with 80mg/day atorvastatin.[5] Taken directly from the results of the trial: "Standard treatment (statin) with a 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitor (pravastatin 40 mg/day) resulted in a 22% reduction in LDL cholesterol levels at 30 days compared with a 51% reduction with intensive therapy (atorvastatin 80 mg/day). At 2 years, a relative risk reduction of 16% (95% confidence interval, 5%-26%; P = 0.005) in the primary end point rate (death, myocardial infarction, documented unstable angina requiring hospitalization, coronary revascularization, or stroke) was seen in patients receiving intensive statin treatment compared with standard statin therapy. The benefit of intensive treatment was apparent as early as 30 days and was consistent over time. The PROVE IT-TIMI 22 data indicate that patients recently hospitalized for an ACS benefit from early and continued lowering of LDL cholesterol to levels substantially below current guideline recommendations."
Adverse effects
Common adverse drug reactions (≥1% of patients) associated with atorvastatin therapy include: myalgia, mild transient gastrointestinal symptoms (diarrhea, constipation, passing gas), elevated hepatic transaminase concentrations, headache, insomnia, joint pain, and/or dizziness.[4]. Myopathy and rhabdomyolysis occur in <0.1% of patients. Risk is increased in patients with renal impairment, serious concurrent illness; and/or concomitant use of drugs which inhibit CYP3A4.[4]
References
- Loftus, Peter. "Pfizer's Lipitor Patent Reissue Rejected", The Wall Street Journal Online, 2007-08-16. Retrieved on 2007-08-27.
- Saul, Stephanie; Alex Berenson (2007-11-03). Maker of Lipitor Digs In to Fight Generic Rival. The New York Times.
- Hawkes, Nigel (2007-10-11). Statins are the right prescription. The Times (UK). Retrieved on 2007-11-03.
- Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006. ISBN 0-9757919-2-3
- Rouleau J (2005). "Improved outcome after acute coronary syndromes with an intensive versus standard lipid-lowering regimen: results from the Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis in Myocardial Infarction 22 (PROVE IT-TIMI 22) trial". Am. J. Med. 118 Suppl 12A: 28-35. doi:10.1016/j.amjmed.2005.09.014. PMID 16356805.
- BBC News, Patent ruling hits Ranbaxy shares, 19 December 2005
- Duncan Bucknell, The global Lipitor patent scorecard, retrieved 2007-03-03
- Zhou Z, Rahme E, Pilote L (2006). "Are statins created equal? Evidence from randomized trials of pravastatin, simvastatin, and atorvastatin for cardiovascular disease prevention". Am. Heart J. 151 (2): 273-81. doi:10.1016/j.ahj.2005.04.003. PMID 16442888.
Selective serotonin reuptake inhibitors (SSRIs)
Molecules of Life Resources
The Cannabidiol Molecule
Cannabidiol (CBD is the major non-psychoactive component of Cannabis and is being looked at by major drug and consumer companies for various medical and social uses.